In anesthesiology, the prevention of healthcare-associated infections (HCAI) has been discussed for decades (1) and the use of breathing filters has been recommended for the prevention of tuberculosis, influenza, and hepatitis C. (2-6)
COVID‐19: Societies recommend the use of breathing filters
Since 2020, the world has been facing an unprecedented healthcare crisis caused by a pandemic novel beta coronavirus, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). In terms of the COVID‐19 pandemic, national and international societies have been quick to cotton on to the continuing situation. Organizations like The European Resuscitation Council, the British NHS, the US American Anesthesia Patient Safety Foundation, and the Safe Airway Society of Australia / New Zealand have all stressed the importance of placing "high quality" airway filters between the breathing circuit and the patient’s airways to "prevent circuit contamination and minimize aerosolization in expired gas" — in short, to minimize the risk of virus spread.(7-10)
Expert opinion survey: What is the most important filter quality?
We conducted a survey and let 200 experts from France, Germany, the UK, and the USA have their say: Clinicians (anesthesiologists, intensive care specialists, anesthesia tech staff) and admin staff (nurses and managers) in the operating room and on the ICU stated what they would rate as the filters' most important qualities, when they choose one.
The product makes the difference: "Highest bacterial / viral efficiency" is the most important quality
Two thirds (66%) of the respondents answer that the product’s performance makes the difference and is the number one decisive factor when choosing a breathing filter. This is made up of 29% of all respondents believing that the "highest bacterial / viral efficiency" of a filter is especially important and 37% of all respondents valuing additional product performance parameters, including "best resistance to wetting / clogging" (15%), "longest filter life" (14%), and "largest number of times you can nebulize through the filter" (8%).
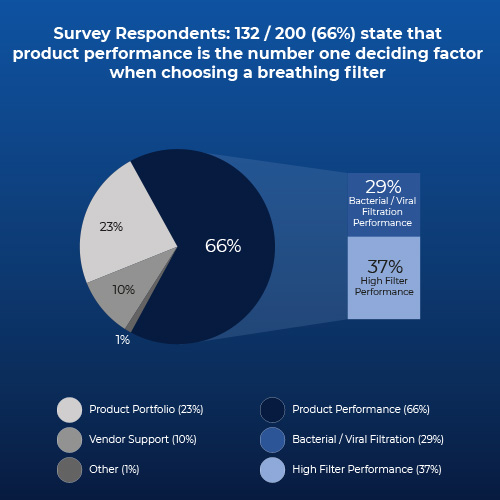
Fig 1. Answers of survey respondents (in %) to the question: What level of importance do you place around each factor when choosing a breathing system filter?
Conclusion
Breathing System Filter users as well as professional organizations acknowledge the need for high efficiency filtration during anesthesia and intensive care ventilation. In laboratory studies as well as in clinical trials, Pall Medical Ultipor™ Breathing System Filters have been shown to retain both airborne microorganisms at >99.999% and liquid borne bacteria and viruses at 100% efficiency, including Influenza A, Hepatitis C, HIV and Mycobacterium tuberculosis.
Download our full check list here and find out more about the validation of our breathing filter.
References
- Zorrilla-Vaca A, Escandón-Vargas K. The importance of infection control and prevention in anesthesiology. Rev Colomb Anestisiol. 2017;45(S 2):69–77. https://doi.org/10.1016/j.rcae.2017.10.001.
- Center for Disease Control (CDC). Guidelines for Preventing the Transmission of Mycobacterium tuberculosis in Health-Care Settings, 2005 Dec 30; 54(RR-17). http://www.cdc.gov/mmwr/pdf/rr/rr5417.pdf. Accessed [2020 Aug 19].
- Sprung CL, Zimmerman JL, Christian MD, Joynt GM, Hick JL, Taylor B, et al. Recommendations for intensive care unit and hospital preparations for an influenza epidemic or mass disaster: summary report of the European Society of Intensive Care Medicine’s Task Force for intensive care unit triage during an influenza epidemic or mass disaster. Intensive Care Med. 2010;36(3):428-443. doi:10.1007/s00134-010-1759-y.
- Blood Borne Viruses Advisory Panel. A Report Received by Council of the Association of Anaesthetists on Blood Borne Viruses and Anaesthesia: An Update (January 1996). London: The Association of Anaesthetists of Great Britain and Ireland, 1996.
- Association of Anaesthetists of Great Britain and Ireland. Infection Control in Anaesthesia. London: The Association of Anaesthetists of Great Britain and Ireland, 2002.
- Association of Anaesthetists of Great Britain and Ireland. Infection control in anaesthesia. Anaesthesia. 2008;63(9): 1027-1036. doi:10.1111/j.1365-2044.2008.05657.x.
- National Health Service. Guidance for the role and use of non-invasive respiratory support in adult patients with COVID19 (confirmed or suspected). NHS. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/specialty- guide-NIV-respiratory-support-and-coronavirus-v3.pdf. Accessed [2020 Aug 19].
- Safe Airway Society. Consensus statement: Safe Airway Society principles of airway management and tracheal intubation specific to the COVID-19 adult patient group. https://www.mja.com.au/journal/2020/consensus-statement-safe-airway- society-principles-airway-management-and-tracheal. Accessed [2020 Aug 19].
- Anesthesia Patient Safety Foundation. FAQ ON ANESTHESIA MACHINE USE, PROTECTION, AND DECONTAMINATION DURING THE COVID-19 PANDEMIC. https://www.apsf.org/faq-on-anesthesia-machine-use-protection-and- decontamination-during-the-covid-19-pandemic/. Accessed [2020 Aug 19].
- European Resuscitation Council. European Resuscitation Council COVID-19 Guidelines. https://www.erc.edu/sites/5714e77d5e615861f00f7d18/pages/5e9ac62b4c84867335e4d1e b/files/ERC_covid19_pages.pdf?1591110476. Accessed [2020 Aug 19].
- Kramer A, Kranabetter R, Rathgeber J, Züchner K, Assadian O, Daeschlein G, et al. Infection prevention during anaesthesia ventilation by the use of breathing system filters (BSF): Joint recommendation by German Society of Hospital Hygiene (DGKH) and German Society for Anaesthesiology and Intensive Care (DGAI). GMS Krankenhaushyg Interdisz. 2010;5(2):Doc13. Published 2010 Sep 21. doi:10.3205/dgkh000156.
Author bio
Dr. Volker Luibl, MBA

Dr. Luibl is a Demand Generation Marketing Manager at Cytiva with knowledge in medical devices and clinical science.