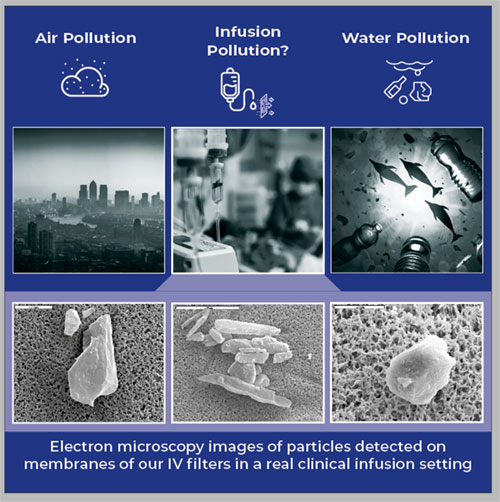
It has become accepted wisdom that air and water particle pollution affects our health daily. To reduce or prevent the risk of particles in air and water, regulators have taken the first step towards quantifying the risk to people's health by measuring exposure.
Almost every city in the world today records and publishes daily levels of particles in the air (1) and the 'California State Water Resources Control Board' is the world's first regulatory authority to announce standard methods for quantifying microplastic concentrations in drinking water (2).
Around 15 years ago, clinicians and researchers started to voice their concerns about the number of particles that are below the regulated sizes in infusion therapy. These are likely to affect the most vulnerable patients of all – those on the intensive care unit (ICU).
Chapter <788> of the United States Pharmacopeia (USP), Particulate Matter in Injections, defines particulate matter as "mobile undissolved particles, other than gas bubbles, unintentionally present in the solutions" (3).
This blog focuses on current knowledge regarding particles associated with water and air pollution and compares this knowledge to what we know about particles in infusion therapy – or simply called "infusion pollution."
Comparison of particle uptake from air, water, and intravenous infusions
To evaluate the quality of air, health departments measure fine particulate matter (PM2.5): teeny tiny particles or droplets with a diameter of 2.5 microns (= µm, a thousandth of a millimeter) or less (to compare: The average hair is 50µm thick). How many PM2.5 you inhale depends on where you live: In London, it may be around 44 million particles per day, in Beijing, up to 220 million per day (4).
In the oceans, the most predominant microplastic particles range in size from 150 to 500 µm (5); on average, each of us consume anywhere between 518 to 3078 microplastic items per year just by eating fish (6).
In much the same vein as in water and air, medical researchers started counting the number of particles that are infused into ICU patients (7, 8 ,9). The results allow for two conclusions. One, the more volume is infused into a patient, the more particles are infused. Two, the number of particles depends strongly on the size of particles: The smaller the particles, the more are infused into the ICU patient. Some recent studies have shown.
- NICU (neonatal ICU) patients receive 85 000 particles > 1 µm in a 24 h infusion period (7)
- PICU (pediatric ICU) patients receive 416 974 particles > 1µm in a 24 h infusion period (8)
- PICU patients receive 25 000 000 000 particles with a size < 1µm in a 24 h infusion period (9).
Conclusion:
The sheer number of particles infused into ICU patients may come as a surprise and can only serve to reinforce the validity of the concerns about their potential impact on the health of our ICU patients.
Comparison of death numbers, health effects and pathologies associated with particles from air, water, and intravenous infusions
According to the World Health Organization (WHO), exposure to ambient (outdoor) air pollution causes 4.2 million deaths per year (10). In the United States alone, PM2.5 is the largest environmental risk factor, resulting in >100 000 premature deaths per year – more than traffic accidents and homicides combined (11). The exposure to PM2.5 is a major risk factor for both mortality and morbidity, with associations demonstrated for everything from asthma over lung cancer to heart attack and stroke, atherosclerosis, thrombosis, hypertension, and arrhythmia; more recently, type 2 diabetes, dementia, and loss of cognitive function were added to this already depressively long list (10–15).
In the oceans, plastic debris causes the deaths of more than a million seabirds and more than 100 000 marine mammals per year (16). In humans, data indicate that microplastics can induce cellular damage, immune responses, neurotoxic and even metabolic changes (17,18,19). Further, microplastic has been now for the first time documented in the placentas of unborn babies, which is of major concern (20).
And what do we know about intravenously infused particles? Over the last 15 years, studies have demonstrated that infused particles can block blood vessels, have systemic hypercoagulability effects, impair microcirculation, and have immune-modulatory and inflammatory effects (21-31). Clinical studies on IV in-line filters have suggested that infused particles are associated with multi-organ failure, systemic inflammatory response syndrome, as well as renal, hematologic, and respiratory dysfunction (32-38). To what extent infused particles cause or contribute to deaths of ICU patients is so far unknown. However, one study did reveal a statistical trend towards lower mortality in those pediatric ICU patients in whom particles were removed with an IV in-line filter before the infusion entered the blood stream (28).
Conclusion:
Inflammatory and immune-modulatory processes seem to be the common and underlying reactions in all three particle-associated pathologies.
Comparison of the chemical composition of particles in air, water, and intravenous infusions
In urban environments, carbon also plays a major part, followed by non-carbon constituents such as minerals, ammonium, nitrates, or sulfates. (39,40)
Most microplastics floating in the ocean are polyethylene, the rest are made up of various other forms of plastic, including polypropylene, polystyrene, and polyester.(19)
Particles infused into ICU patients range from various plastics to titanium oxide and silicon oil. (41) The main source of these particles is the infusion equipment; other causes might be drug incompatibilities (42,43), ampoules (glass particles) (44) and foreign particles in drug products, such as cellulose fibers. (41)
Conclusion:
Particles in air are rather different in their chemical composition in comparison to particles in water and infusions.
Comparison of our natural defenses for the prevention of particles entering the bloodstream
According to a report from the World Wildlife Fund (WWF) combining the results of more than 50 studies worldwide, people could on average be ingesting about 5 g of particles every week. That is the equivalent of one credit card that we take in through the air we breathe, the food we eat, and the water we drink (45).
Fortunately, not all particles reach the blood stream, since healthy lungs, gut and skin normally function as effective biological barriers. Regarding air particles, our natural defenses help us to cough or sneeze some coarse particles out of our bodies.
By contrast, particles in infusions can enter the bloodstream directly without any natural defense – unless an IV in-line filter prevents them from doing so.
Conclusion:
Particles that we breathe and particles that we drink or ingest may be prevented from entering the bloodstream via the lung and gut, but particles that we infuse enter the bloodstream without any barrier.
Comparison of guidelines and policies fighting particle pollution in air, water, and intravenous infusions
In 2012, the U.S. Environmental Protection Agency (EPA) strengthened the nation's air quality standards for fine particle pollution by revising the primary annual PM2.5 standard to 12 µg per cubic meter (µg/m3) (46). The European Union (EU) Clean Air Directive is currently among the strictest acts of legislation worldwide concerning PM10 air pollution. Its most visible result has been the rapid adoption of "Low Emission Zones" (LEZs), which define areas that vehicles may only enter if they are classified as low PM10 emitting vehicles (47). The World Health Organization has set a target for cities to achieve an average of 10 micrograms of PM2.5 per cubic meter (48).
So, what have regulators been doing against this particle tidal wave? As you might expect, lots of international and national meetings have resulted in goals and policies to decrease the amount of microplastics in water. Amongst these was the G20 Osaka Summit in 2019 with its "Osaka Blue Ocean Vision," aiming to reduce additional pollution by marine plastic litter to zero by 2050; all G20 leaders called on other members of the international community to share this vision (49). What else? For example, California is set to establish the first ever health-based guidelines for acceptable levels of microplastics in drinking water (50).
So, what about policies that aim to minimize the risk of particle harm to patients via infusions? Well, standards and regulations do exist today to control particle contaminations of injectable products. For example, both the United States Pharmacopoeia (USP) and the European Pharmacopeia (EP) have chapters on particulate contamination, and both set limits for the number of particles (≥10 µm and ≥25 µm) allowed to be contained in injectable drugs.(51, 52) Apart from pharmacopeias, manufacturers also face rules: They must ensure the absence of any contaminants such as glass fragments in accordance with Good Manufacturing Practices (GMPs) to obtain quality products (52).
Conclusion:
Regulators are aware of the potential risk of particles to humans, and tremendous efforts are made to minimize this risk.
Comparison of potential measures to prevent particle uptake from air, water, and intravenous infusions
Various organizations have handed out practical advice. For instance, the 'American Lung Association' instigated the 'Healthy Air Campaign,' encouraging everyone to check daily air pollution forecasts in their area, avoid outdoor exercise during high pollution levels and to generally walk, bike, or carpool instead of driving (53). Protective face masks are another option: The most effective ones filter up to 95% of airborne particles (down to 0.3 µm) (54). In China and other Asian countries with severe air pollution, wearing a mask was common before the Corona pandemic started and has now increased even more (54). Besides wearing a face mask, you may consider relocation. As a US citizen you may decide to move to South Burlington in Vermont, which boasts the cleanest air in the United States (55).
Protecting yourself from microplastic in the ocean might be difficult, but technologies to improve household drinking water do exist, which include point-of-use and point-of-entry filters (56).
Drug manufacturers control the risk of particles by recommending the use of IV in-line filters for specific drugs in their instructions for use. The recently updated chart of IV drugs to be used with a syringe or with an in-line filter, published in 'Hospital Pharmacy,' offers an extensive list of different drug categories, including monoclonal antibody formulations, antimicrobial drugs, cancer drugs, and more (57). Besides drug manufacturers, medical societies such as ASPEN and INS (American Society for Enteral Nutrition, Infusion Nurses Society) also attempt to minimize the risk of particles by recommending the use of in-line filters (58,59).
Conclusion:
Research is the crucial factor to enable authorities to make rational decisions on how we can protect us from particle risks. Besides that, we all need to be aware of the risks and must act accordingly.
Summary
"Particles affect human health as a function of their properties such as chemical composition, size and shape, but also depending upon complex interactions in a living organism that occur at various levels between uptake of the particle and responses of the target organ" (60).
While the public is mostly aware of air and water pollution, researchers have expressed increased concerns about the health impact of infusion pollution on ICU patients. This is an issue that surely deserves more attention, with the goal of protecting our patients.
In a nutshell: particles do matter for the air we breathe, do matter for the water we drink, and do matter for the infusions we give.
- IQAIR. Air quality in the world. https://www.iqair.com/world-air-quality. Accessed [2022 Mar 1].
- Cal Matters. Premature or precautionary? California is first to tackle microplastics in drinking water. https://calmatters.org/environment/2021/03/california-microplastics-drinking-water/. Accessed [2022 Mar 1].
- Langille SE. Particulate Matter in Injectable Drug Products. PDA J Pharm Sci Technol. 2013;67(3):186-200.
- U-Earth Team. How much pollution do you breathe in every day? https://www.u-earth.eu/post/how-much-pollution-breathe-every-day. Accessed [2022 Mar 1].
- Alfaro-Núñez A, Astorga D, Cáceres-Farías L, Bastidas L, Soto Villegas C, Choez Macay K, et al. Microplastic pollution in seawater and marine organisms across the Tropical Eastern Pacific and Galápagos [published correction appears in Sci Rep, 2021;11(1):6424. Published 2021 Mar 19. doi.org/10.1038/s41598-021-85939-3.
- Barboza LGA, Guilherminio L. Microplastics in wild fish from North East Atlantic Ocean and its potential for causing neurotoxic effects, lipid oxidative damage, and human health risks associated with ingestion exposure. Science of The Total Environment. 2020;717:134625. https://doi.org/10.1016/j.scitotenv.2019.134625.
- Perez M, Décaudin B, Maiguy-Foinard A, Barthélémy C, Lebuffe G, Storme L, et al. Dynamic Image Analysis To Evaluate Subvisible Particles During Continuous Drug Infusion In a Neonatal Intensive Care Unit. Sci Rep. 2017;7(1):9404. Published 2017 Aug 24. Doi:10.1038/s41598-017-10073-y.
- Perez M, Décaudin B, Abou Chahla W, Nelken B, Storme L, Masse M, et al. Effectiveness of in-Line Filters to Completely Remove Particulate Contamination During a Pediatric Multidrug Infusion Protocol. Sci Rep. 2018;8(1):7714–. Published 2018 May 16. Doi:10.1038/s41598-018-25602-6.
- Keck, C.M. et al. (2016). How Many Nanoparticles Enter a Patient during infusion therapy? J Vasc Access; 17(4): 100 (O-26)
- World Health Organization (WHO). Air pollution. https://www.who.int/health-topics/air-pollution#tab=tab_1. Accessed [2022 Mar 1].
- Goodkind A, Tessum CW, Coggins JS, Hill JD, Marshall JD. Fine-scale damage estimates of particulate matter air pollution reveal opportunities for location-specific mitigation of emissions. Proc Natl Acad Ssci U S A. 2019;116(18):8775-8780. doi:10.1073/pnas.1816102116.
- Loxham M, Nieuwenhuijsen MJ. Health effects of particulate matter air pollution in underground railway systems – a critical review of the evidence. Part Fibre Toxicol. 2019; 16(1):12. Published 2019 Mar 6. doi:10.1186/s12989-019-0296-2.
- Hamanaka RB, Mutlu GM. Particulate Matter Air Pollution: Effects on the Cardiovascular System. Frontiers in Endocrinology. Front Endocrinol (Lausanne). 2018;9:680. Published 2018 Nov 16. doi:10.3389/fendo.2018.00680.
- United States Environmental Protection Agency (U.S. EPA).How Does PM Affect Human Health? https://www3.epa.gov/region1/airquality/pm-human-health.html. Accessed [2022 Mar 2].
- Leni Z, Cassagnes LE, Daellenbach KR, El Haddad I, Vlachou A, Uzu G, et al. Oxidative stress-induced inflammation in susceptible airways by anthropogenic aerosol. PLOS One. 2020;15(11):e0233425. Published 2020 Nov 18. doi.org/10.1371/journal.pone.0233425.
- The Ocean Conference. https://sustainabledevelopment.un.org/content/documents/Ocean_Factsheet_Pollution.pdf. Accessed [2022 Mar 2].
- Yong CQY, Valiyaveettil S, Tang BL. Toxicity of Microplastics and Nanoplastics in Mammalian Systems. Int J Environ Res Public Health. 2020;17(5):1509. https://doi.org/10.3390/ijerph17051509.
- Frontier. Microplastics in Water and Potential Impacts on Human Health. https://www.frontiersin.org/research-topics/22088/microplastics-in-water-and-potential-impacts-on-human-health. Accessed [2022 Mar 3].
- Issac MN, Kandasubramanian B. Effect of microplastics in water and aquatic systems. Environ Sci Pollut Res Int. 2021;28(16):19544-19562. doi:10.1007/s11356-021-13184-2.
- Ragusa A, Svelato A, Santacroce C, Catalano P, Notarstefano V, Carnevali O, et al. First evidence of microplastics in human placenta. Environ Int. 2021;146:106274. doi.org/10.1016/j.envint.2020.106274.
- Ilium L, Davis SS, Wilson CG, Thomas NW, Frier M, Hardy JG. Blood clearance and organ deposition of intravenously administered colloidal particles. The effects of particle size, nature and shape. Int J Pharm. 1982;12(2-3):135-146. https://doi.org/10.1016.0378-5173(82)90113-2.
- Bradley JS, Wassel RT, Lee L Nambiar S. Intravenous ceftriaxone and calcium in the neonate: assessing the risk for cardiopulmonary adverse events. Pediatrics. 2009; 123(4):e609-613. doi:10.1542/peds.2008-3080.
- Puntis JWL, Wilkins K, Ball P, Rushton D, Booth I. Hazards of parenteral treatment: do particles count? Archives of Disease in Childhood. 1992;67:1475-1477. doi:10.1136/adc.67.12.1475.
- Boehne M, Jack T, Kӧditz H, Seidemann K, Schmidt F, Abura M, et al. In-line filtration minimizes organ dysfunction: New aspects from a prospective, randomized, controlled trial. BMC Pediatrics. 2013;13(21):1-8.
- Kirkpatrick CJ, Rangoonwala R, Reshetnykov M, Barback M, Ghanaati S. Non-Equivalence of Antibiotic Generic Drugs and Risk for Intensive Care Patients. Pharmaceut Reg Affairs. 2013;2(1):1-7. doi:10.4172/2167-7689.1000109.
- Schaefer SC, Bison PA, Rangoonwala R, Kirkpatrick CJ. Lehr H-A. 0.2 µm in-line filters prevent capillary obstruction by particulate contaminants of generic antibiotic preparations in postischemic muscle. Chemother J. 2008;17(4): 172-178.
- Lehr HA, Brunner J, Rangoonwala R, Kirkpatrick CJ. Particulate Matter Contamination of Intravenous Antibiotics Aggravates Loss of Functional Capillary Density in Postischemic Striated Muscle. Am J Respir Crit Care Med. 2002;165:514-520. doi:1.1164/AJRCCM.165.4.210833.
- Jack T, Boehne M, Brent B, Hoy L, Kӧditz H, Wessel A, et al. In-line filtration reduces severe complications and length of stay on pediatric intensive care unit: a prospective, randomized, controlled trial. Intensive Care Med. 2012;38:1008-1016.
- Jack T, Brent BE, Boehne M, Müller M, Sewald K, Braun A, et al. Analysis of particulate contaminations of infusion solutions in a pediatric intensive care unit. Intensive Care Med. 2010;36:707-711.
- Schmitt E, Meybohm P, Herrmann E, Ammersbach K, Endres R, Lindau S, et al. In-line filtration of intravenous infusion may reduce organ dysfunction of adult critical patients. Crit Care. 2019;23(373). Published 2019 Nov 22. doi:10.1186/s13054-019-2618-z.
- Chisholm CF, Behnke W, Pokhilchuk Y, Frazer-Abel AA, Randolph TW. Subvisible Particles in IVIg Formulations Activate Complement in Human Serum. J Pharm Sci. 2020;109(1):558-565. doi:10.1016/j.xphs.2019.10.041.
- Schaefer SC, Bison PA, Rangoonwala R, Kirkpatrick CJ, Lehr H-A. 0.2 µm in-line filters prevent capillary obstruction by particulate contaminants of generic antibiotic preparations in postischemic muscle. Chemother J. 2008;17(4):172-178.
- Jack T, Boehne M, Bernadette EB, Hoy L, Kӧditz H, Wessel A, et al. In-line filtration reduces severe complications and length of stay on pediatric intensive care unit: a prospective, randomized, controlled trial. Intensive Care Med. 2012;38:1008-1016.
- Boehne M, Jack T, Kӧditz H, Seidemann K, Schmidt F, Abura M, et al. In-line filtration minimizes organ dysfunction: New aspects from a prospective, randomized, controlled trial. BMC Pediatrics. 2013;13 (21):1-8.
- Sasse M, Dziuba F, Jack T, Kӧditz H, Kaussen T, Bertram H, et al. In-line Filtration Decreases Systemic Inflammatory Response Syndrome, Renal and Hematologic Dysfunction in Pediatric Cardiac Intensive Care Patients. Pediatr Cardiol. 2015;36(6):1270-1278. doi: 10.1007/s00246-015-1157-x.
- Villa G, Chelazzi C, Giua R, Tofani L, Zagli G, Boninsegni P, et al. In-Line Filtration Reduces Postoperative Venous Peripheral Phlebitis Associated With Cannulation: A Randomized Clinical Trial. Anesth Analg. 2018;127(6):1367-1374. doi:10.1213/ANE.0000000000003393.
- Schmitt E, Meybohm P, Herrmann E, Ammersbach K, Endres R, Lindau S, et al. In-line filtration of intravenous infusion may reduce organ dysfunction of adult critical patients. Critical Care. 2019;23(1):373. Published 2019 Nov 22. doi:10.1186/s13054-019-2618-z.
- Virlouvet AL, Pansiot J, Toumazi A, Colella M, Capewell A, Guerriero E, et al. In-line filtration in very preterm neonates: a randomized controlled trial. Sci Rep. 2020;10 (1):5003. Published 2020 Mar 10. doi:10.1038/s41598-020-61815-4.
- Philip S, Martin RV, Donkelaar van A, Lo JW-H, Wang Y, Chen D, et al. Global Chemical Composition of Ambient Fine Particulate Matter for Exposure Assessment. Environ Sci Technol. 2014;48(22):13060-13068. doi:10.1021/es502965b.
- Miller MR. Oxidative stress and the cardiovascular effects of air pollution. Free Radic Biol Med. 2020;151:69-87. doi:10.1016/j.freeradbiomed.2020.01.004.
- Pittiruti M, Sasse M, Braun A, Keck C, Lankers M, Muñoz PG, et al. Time to rethink filtration. British Journal of Nursing. 2016;25(19). Published 2016 Nov 9. https://doi.org/10.12968/bjon.2016.25.Sup19.1.
- Gikic M, Di Paolo ER, Pannatier A, Cotting J. Evaluation of physicochemical incompatibilities during parenteral drug administration in a paediatric intensive care unit. Pharm World Sci. 2000;22(3):88-91. doi:10.1023/a:1008780126781.
- Sriram S, Aishwarya S, Moithu A, Sebastian A, Kumar A. Intravenous Drug Incompatibilities in the Intensive Care Unit of a Tertiary Care Hospital in India: Are they Preventable? J Res Pharm Pract. 2020;9(2):106-111. Published 2020 Jun 26. doi:10.4103/jrpp.JRPP_20_11.
- Joo GE, Sohng K-Y, Park MY. The effect of different methods of intravenous injection on glass particle contamination from ampules. SpringerPlus. 2016;5(15).
- WWF 2019. No Plastic in Nature: assessing plastic ingestion from nature to people. https://wwf.fi/app/uploads/9/3/m/urcue1dmjetxn1otmy2wc0/plastic-ingestion-raportti-wwf.pdf. Accessed [2022 Mar 2].
- United States Enrivonmental Protection Agency (U.S. EPA). REVISED AIR QUALITY STANDARDS FOR PARTICLE POLLUTION AND UPDATES TO THE AIR QUALITY INDEX (AQI). https://www.epa.gov/sites/default/files/2016-04/documents/2012_aqi_factsheet.pdf. Accessed [2022 MNar 2].
- Wolff H Perry L. Trends in Clean Air Legislation in Europe: Particulate Matter and Low Emission Zones. The University of Chicago Press Journals. 2010;4(2). doi.org/10.1093/reep/req008.
- World Health Organization (WHO) 2021. Ambient (outdoor) air pollution. https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health. Accessed [2022 Mar 2].
- MICHIDA Y. Guidelines for Harmonizing Ocean Surface Microplastic Monitoring Methods. Ministry of the Environment Japan.2019:71. https://www.env.go.jp/en/water/marine_litter/guidelines/guidelines.pdf.
- Mosko S. Why California’s First-in-World Plan to Monitor Microplastics in Drinking Water Matters. Fullerton Observer. 2021. https://fullertonobserver.com/2021/04/21/why-californias-first-in-world-plan-to-monitor-microplastics-in-drinking-water-matters/.
- Langille SE. Particulate matter in injectable drug products. PDA J Pharm Sci Technol. 2013;67(3):186-200. doi:10.5731/pdajpst.2013.00922.
- Perez M, Maiguy-Foinard A, Barthélémy C, Décaudin B, Odou P. Particulate Matter in Injectable Drugs: Evaluation of Risks to Patients. Pharmaceutical Technology in Hospital Pharmacy. 2016;1(2):91-103. https://doi.org/10.1515/pthp-2016-0004.
- American Lung Association. 10 Tips to Protect Yourself from Unhealthy Air. https://www.lung.org/clean-air/outdoors/10-tips-to-protect-yourself. Accessed [2022 Mar 3].
- IQAir. Air pollution masks: What works, what doesn’t. https://www.iqair.com/us/blog/air-quality/air-pollution-masks-what-works-what-doesn-t. Accessed [2022 Mar 3].
- Stacker. U.S. cities with the cleanest air. https://stacker.com/stories/3291/us-cities-cleanest-air. Accessed [2022 Mar 3].
- Center for Disease Control (CDC). A Guide to Drinking Water Treatment Technologies for Household Use. https://www.cdc.gov/healthywater/drinking/home-water-treatment/household_water_treatment.html. Accessed [2022 Mar 3].
- Ipema HJ, Zacher JM, Galka E, Nazari J, Varabyeva A, Yu M. Drugs to Be Used With a Filter for Preparation and/or Administration-2019. Hosp Pharm. 2021;56(2):81-87. doi:10.1177/0018578719867660.
- Gorski LA, Hadaway L, Hagle ME, Broadhurst D, Clare S, Kleidon T, et al. Infusion Therapy Standards of Practice, 8th Edition. J Infus Nurs. 2021; 44(1S Suppl 1):S1-S224. doi:10.1097/NAN.0000000000000396.
- Worthington P, Gura KM, Krast MD, Nishikawa R, Guenter P, Sacks GS, et al. Update on the Use of Filters for Parenteral Nutrition: An ASPEN Position Paper. Nutr Clin Pract. 2020;36(1):29-39. doi:10.1002/ncp.10587.
- Riediker M, Zink D, Kreyling W, Oberdӧrster G, Elder A, Graham U, et al. Particle toxicology and health - where are we? Part Fibre Toxicol. 2019;16(19):1-33. Published 2019 Apr 23. doi:10.1186/s12989-019-0302-8.
Author bio
Dr. Volker Luibl, MBA

Dr. Luibl is a demand generation marketing manager with knowledge in medical device and clinical science.