Pseudomonas aeruginosa in Drinking Water
Pseudomonas aeruginosa (PA) is a Gram-negative bacillus which, is tolerant of a wide variety of physical conditions, has minimal nutrition requirements, and is a major opportunistic pathogen. PA appears sporadically in drinking water distribution systems, but seems to occur at a higher frequency in premise plumbing systems compared to water mains.
PA is one of the most common and problematic bacteria in healthcare facilities, and is responsible for approximately 10-20 % of hospital-associated infections (HAI) (pneumonia, wound infections, blood stream infections and urinary tract infections) in intensive care units (ICUs). Length of stay, severity of underlying disease and exposure to invasive procedures, bacterial adherence, virulence factors, and antimicrobial drug resistance are associated with PA infections in ICUs. The incidence of HAI is 5 - 10 times higher in ICU than general wards 4.
Although endogenous origin was considered as the most relevant route of PA infections, in the last ten years a significant proportion of PA isolates have been shown to stem from the ICU environment and cross-transmission5,6. Several studies have shown that up to 50 % of hospital acquired PA infections may be derived from the in-premise water distribution system3,7,8. Unlike patient and pathogen characteristics, environmental factors such as nursing workload or contamination of water outlets can be more easily managed and modified.
PA can colonize many types of fluids (even distilled water) and rapidly forms biofilms1,5,9-12. Moreover, PA can thrive in water fittings including the faucet body, connectors and flow straighteners, sinks, drains, toilets, shower heads and hoses. Automatic sensor faucets have been shown to be more likely to become contaminated than non-sensor manual outlets10.
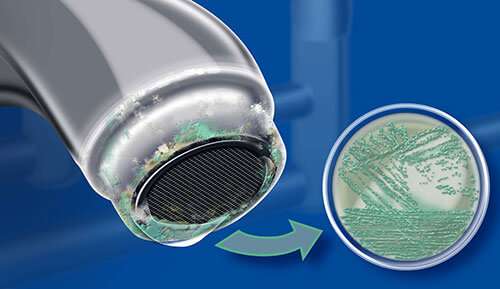
Pseudomonas aeruginosa may colonize biofilms in water systems and be released from the outlet.
Pseudomonas aeruginosa may colonize flow straighteners and aerators as well as bottled water.
Pseudomonas aeruginosa has been observed growing within drinking water biofilms2,13, thus protected and more difficult to eradicate than planktonic bacteria1,14. PA is resistant to chlorine and other disinfectants used in water treatments1,15 and may survive in the hospital ward environment even after disinfection16, increasing the risk of acquisition by patients17. PA living in biofilms exerts a higher resistance towards disinfectants due to the mechanical protection provided by the biofilm matrix18-20.
It has been shown that the use of sublethal concentrations of chlorine-based oxidizing agents (sodium hypochlorite, chlorine dioxide, electrochemically activated chlorine, continuous treatment with 0.15 ppm chlorine or shock treatment with 10 ppm chlorine for 6 hours (h)) can lead to a cyclical regrowth of biofilm after treatment end and the survival of PA living in the biofilm. Under unfavorable operating conditions in a drinking water system, PA has been shown to survive sequentially 24 h 50 parts per million (ppm) chlorine dioxide (ClO2), 3 minutes 70 °C and 24 h 50 ppm ClO216.
In a large hospital in Taiwan, a comparative study on infection rates with and without continuous treatment with ClO2 has been described. Building 1 was continuously treated (over 11 months) with ClO2, whereas building 2 was not treated. In both cases infections were monitored. The overall rate of non-fermentative Gram-negative bacilli nosocomial infections did not decline after ClO2 disinfection. Furthermore, PA infection rates increased in both buildings, showing no evidence for a relationship between ClO2 treatment and PA infection rates21.
Pseudomonas aeruginosa living within biofilms typically exerts higher resistance towards chemical and thermal disinfection measures than planktonic PA, thus making PA contamination difficult to eradicate in a water system.
Pall Disposable Point-of-Use Water Filters containing double layer, 0.2 micron sterilizing grade Supor® membranes act as a barrier to, and are validated for, removal of waterborne bacteria – including Pseudomonas spp., protozoa, fungi and particles from the drinking water supply. The filters are suitable for various uses including the provision of water for drinking, food production, personal hygiene, showering and bathing. Pall Point-of-Use Water Filters can support the management and control of Pseudomonas risk within buildings. See the Pall Filtration Solutions
참고문헌:
1. Falkinham et al., “Epidemiology and ecology of opportunistic premise plumbing pathogens: Legionella pneumophila, Mycobacterium avium and Pseudomonas aeruginosa”, Environ Health Perspect, 123(8):749-58, 2015
2. Moritz et al., “Integration of Pseudomonas aeruginosa and Legionella pneumophila in drinking water biofilms grown on domestic plumbing materials”, Int J Hyg Environ Health, 213(3):190-7, 2010
3. Mena & Gerba, “Risk assessment of Pseudomonas aeruginosa in water”, Rev Environ Contam Toxicol, 201:71-115, 2009
4. Cornejo-Juárez et al., “The impact of hospital-acquired infections with multidrug-resistant bacteria in an oncology intensive care unit”, Int J Infect Dis, 31:31-4, 2015
5. Rogues et al., “Contribution of tap water to patient colonisation with Pseudomonas aeruginosa in a medical intensive care unit”, J Hosp Infect, 67:72-8, 2007
6. Kossow et al., “Control of multidrug resistant Pseudomonas aeruginosa in allogeneic hematopoietic stem cell transplant recipients by a novel vundle including re-modelling of sanitary and water supply systems.” Clin Infect Dis, 2017
7. Cholley et al., “The role of water fittings in intensive care rooms as reservoirs for the colonisation of patients with Pseudomonas aeruginosa”, Intensive Care Med 34:1428-33, 2008
8. Cohen et al., “Water faucets as a source of Pseudomonas aeruginosa infection and colonisation in neonatal and adult intensive care unit patients.” Am J Infect Control, 45(2):206-9. 2017
9. Loveday et al., “Association between healthcare water systems and Pseudomonas aeruginosa infections: a rapid systematic review”, J Hosp Infect, 86(1):7-15, 2014
10. Walker et al., “Investigation of healthcare acquired infections associated with Pseudomonas aeruginosa biofilms in taps in neonatal units in Northern Ireland”, J Hosp Infect, 86(1):16-23, 2014
11. Walker & Moore, “Pseudomonas aeruginosa in hospital water systems: biofilms, guidelines prachalities”, J Hosp Inf, 89(4):324-7, 2015
12. Masák et al., “Pseudomonas biofilms: possibilities of their control. FEMS Microbiol Ecol, 89(1):1–14, 2014
13. Flemming & Wingender, “The Biofilm Matrix”, Nat Rev Mircobiol, 8(9):623-33, 2010
14. Ashbolt, NJ. Environmental (saprozoic) pathogens of engineered water systems: Understanding their ecology for risk assessment and management. Pathogens, 4(2):390-405. 2015
15. Bédard et al., “Recovery of Pseudomonas aeruginosa culturability following copper- and chlorine-induced stress”, FEMS Microbiol Lttr, 356:226-34, 2014
16. “Erkenntnisse aus dem Projekt “Biofilm-Management”: Erkennung, Risiko und Bekämpfung von vorübergehend unkultivierbaren Pathogenen in der Trinkwasser-Insatllation”, Verbundprojekt der Universitäten Duisburg-Essen, Berlin und Bonn sowie der DVGW-Forschungsstelle TU Hamburg-Harburg und des IWW Zentrum Wasser, Mülheim, 2010-2014, http://iww-online.de/ download/erkenntnisse-aus-dem-projekt-biofilm-management/
17. Wilson et al., “Prevention and control of multi-drug-resistant Gram-negative bacteria: recommendations from a Joint Working Party”, J Hosp Infect 92:S1S44, 2016
18. Schwering et al., “Multi-species biofilms defined from drinking water microorganisms provide increased protectoin against chlorine disinfection”, Biofouling, 29(8):917-28, 2013
19. Sanchez-Vizuete et al.,“Pathogens protection against the action of disinfectants in multispecies biofilms”, Front Microbiol, 6, 705, 2015
20. Kekeç et al., “Effects of chlorine stress on Pseudomonas aeruginosa biofilm and analysis of related gene expressions”. Curr Microbiol, 73(2):228-35, 2016
21. Hsu et al., “Efficacy of chlorine dioxide disinfection to non-fermentative Gramnegative bacilli and non-tuberculous mycobacteria in a hospital water system”, J Hosp Infect, 93(1):22-8, 2016
This site is intended for U.S. audiences only. Please consult your sales representative or customer support for product availability.