Explore the Benefits & Solutions of Air Eliminating Filtration
“The culture of “a little air won’t hurt you” is as outdated as the Model T Ford and it is time to stop perpetuating this misguided belief on future generations of health care workers.”1
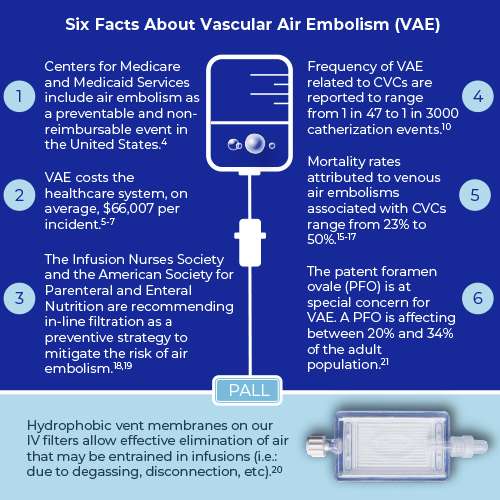
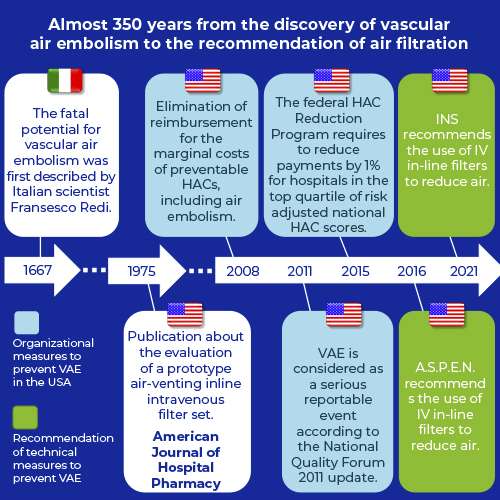
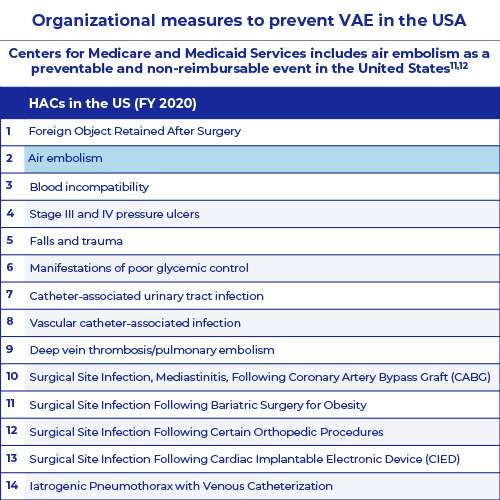
Air embolism is a preventable hospital-acquired condition (HAC) that can result in serious harm, including death.2,3 HAC is a medical diagnose that a patient can develop during a hospital stay that was not present on admission.3 In 2008, a provision of the Deficit Reduction Act of 2005 known as Medicare “Nonpayment” went into effect, eliminating reimbursement for the marginal costs of preventable HACs, including air embolism.4
Therefore, preventing the entrance of air into the patient’s circulatory system can result in tangible budget savings for healthcare providers. Incidences of vascular air embolism (VAE), when one or more air bubbles enter a vein and block it, costs the healthcare system, on average, $66,007 per incident.5-7
Within the hospital environment there are multiple ways air may enter the venous circulation, such as surgical procedures, pain management procedures, diagnostic procedures, hemoperfusion and air from intravenous infusion therapy.8 Regarding VAE, central venous catheters (CVC) warrants special attention. Approximately eight percent of hospitalized patients require central venous access, e.g. more than five million CVCs are inserted in the United States each year.9
Estimates of the frequency of VAE related to CVCs vary from study to study and are reported to range from 1 in 47 to 1 in 3000 catherization events or from 0.1% to 2% per patient.10-14 According to a Pennsylvania Patient Safety Authority report, 41% of VAEs are associated with central venous access devices.2
While the frequency of this complication may be low, mortality rates attributed to venous air embolisms associated with CVCs range from 23% to 50%.15-17
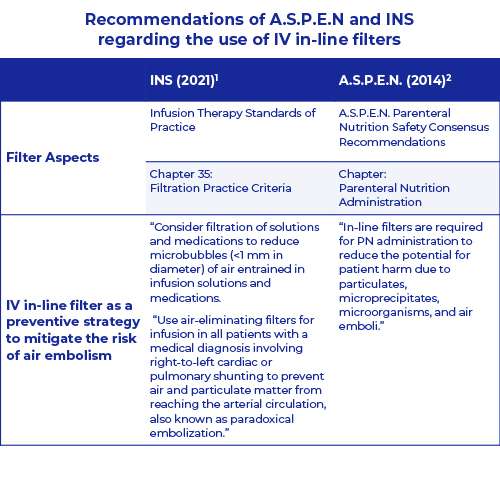
Technical measures, such as the use of an air-eliminating filter, play a crucial role for healthcare providers to prevent VAE. In this respect, the Infusion Nurses Society and the American Society for Parenteral and Enteral Nutrition are recommending in-line filtration as a preventive strategy to mitigate the risk of air embolism.18,19
In 2021 the INS states the following regarding the use of intravenous (IV) in-line filters:
- “Consider filtration of solutions and medications to reduce microbubbles (<1 mm in diameter) of air entrained in infusion solutions and medications.”
- “Use air-eliminating filters for infusion in all patients with a medical diagnosis involving right-to-left cardiac or pulmonary shunting to prevent air and particulate matter from reaching the arterial circulation, also known as paradoxical embolization.”18
Hydrophobic vent membranes on our IV in-line filters allow effective air elimination that may be entrained in infusions (i.e.: due to degassing, disconnection, etc) and protect against air emboli in patients. Results from internal studies demonstrate that our filters can eliminate entrained air in both a vertical and horizontal position.21 Learn more about air emboli and the use of in-line filters in the following chapters.
References
- Myers G.J. (2017). Air in intravenous lines: a need to review old opinion. Perfusion; 32(6): 432-435
- Feil M. (2012). Reducing Risk of Air Embolism Associated with Central Venous Access Devices. Pennsylvania Patient Safety Authority; 9 (2): 58-65
- Center for Medicare and Medicaid Services. (2020). Publicly Reported DRA HAC Measures - Frequently Asked Questions from https://www.cms.gov/files/document/frequently-asked-questions-publicly-reported-deficit-reduction-act-dra-hospital-acquired-condition.pdf [accessed 02/23/2021]
- Kornkven A. (2020). The Impact of Medicare Nonpayment: A Quasi-Experimental Approach from https://sites.duke.edu/djepapers/files/2020/06/audreykornkven-dje.pdf [accessed 02/23/2021]
- Rowland HT. (2009). When never happens: Implications of Medicare’s never event policy. Marquette Elder’s Advi; 10: 341-82
- Bhananker S.M. et al. (2009). Liability related to peripheral venous and arterial catheterization: A closed claims analysis. Anesth Analg; 109: 124-9
- Domino K.B. et al. (2004). Injuries and liability related to central vascular catheters: A closed claims analysis. Anesthesiology; 100: 1411-8
- Mirski M.A., Lele A.V., M.D., Fitzsimmons L., Toung T.J.K. (2007). Diagnosis and Treatment of Vascular Air Embolism. Anesthesiology; 106: 164-177
- Kornbau C., Lee K.C., Hughes G.D., Firstenberg MS. (2015). Central line complications. Int J Crit Illn Inj Sci; 5(3): 170-178.
- Cook L.S. (2013). Infusion-Related Air Embolism. Journal of Infusion Nursing; 36 (1): 26-36
- Boersma R.S., Jie K.S., Verbon A., van Pampus E.C., Schouten H.C. (2008). Thrombotic and infectious complications of central venous catheters in patients with hematological malignancies. Ann Oncol; 19: 433-442
- Gordy S., Rowell S. (2013). Vascular air embolism. Int J Crit Illn Inj Sci;3 (1): 73-76
- Scott W.L. (1988). Complications Associated with Central Venous Catheters: A Survey. Chest; 94 (6): 1221-1224
- Vesely T.M. (2001). Air Embolism during Insertion of Central Venous Catheters. Journal of Vascular and Interventional Radiology; 12 (11): 1291-1295
- Feil M. (2015). Preventing central line air embolism. Am J Nurs; 115 (6): 64-9.
- Heckmann J.G. et al. (2000). Neurologic manifestations of cerebral air embolism as a complication of central venous catheterization. Crit Care Med; 28(5): 1621-5
- Kashuk J.L., Penn I. (1984). Air embolism after central venous catheterization. Surg Gynecol Obstet; 159: 249-52
- Gorski L.A. et al. (2021). Infusion Therapy Standards of Practice, 8th Edition. J Infus Nurs; 01(44): S1-S224
- Ayers P. et al. (2014) A.S.P.E.N. Parenteral Nutrition Safety Consensus Recommendations. Journal of Parenteral and Enteral Nutrition; 38 (3): 296-333
- Stephens A. (2010). Air Elimination Capabilities of the Pall Lipipor™ TNA2 Filter for Parenteral Nutrition. Pall Technical report # 10.3992
- Giblett J.P., Abdul-Samad O., Shapiro L.M., Rana B.S., Calvert P.A.(2019). Patent Foramen Ovale Closure in 2019. Interv Cardiol;14(1): 34-41.
Thank you
Thank you for your interest. We will be in touch soon.
Air embolism, also called a gas embolism, is a preventable hospital-acquired condition that can result in serious harm, including death.1,2
An air embolism occurs when one or more air bubbles enter a vein or artery and block it.
- It’s called a venous air embolism (VAE) when an air bubble enters a vein,
- It’s called an arterial air embolism when an air bubble enters an artery.3
Basically, venous air embolism occurs when two conditions are met:
- there is direct connection between a source of air and the vascular system and
- the pressure gradient favors the entry of this air into the bloodstream1
It took almost 350 years from the first description of the fatal potential of vascular air embolism (1667) to the recommendation of the use of IV in-line filter as a technical measure to prevent vascular air embolism (2016).
References
- Feil M. (2012). Reducing Risk of Air Embolism Associated with Central Venous Access Devices. Pennsylvania Patient Safety Authority; 9 (2): 58-65
- Center for Medicare and Medicaid Services. (2020). Publicly Reported DRA HAC Measures - Frequently Asked Questions from https://www.cms.gov/files/document/frequently-asked-questions-publicly-reported-deficit-reduction-act-dra-hospital-acquired-condition.pdf [accessed 02/23/2021]
- Healthline (2021). Air Embolism. [Updated 2017 August 15]. Available from: https://www.healthline.com/health/air-embolism#outlook
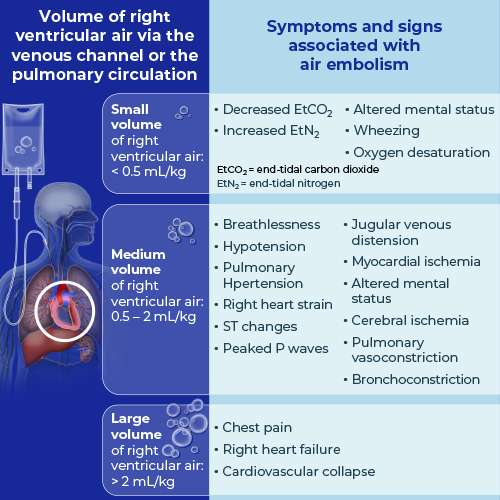
Basically, there are two crucial factors that determine the morbidity and mortality of vascular air embolism (VAE):
- the volume of air entrainment and
- the rate of accumulation1
How much air is lethal?
- Animal studies have demonstrated that approximately 0.5– 0.75 ml/kg of air in rabbits and 7.5–15.0 ml/kg of air in dogs is lethal.2-4
- Case reports of accidental intravascular delivery of air in humans have described the lethal volume as between 200 and 300 ml, or 3–5 ml/kg.5,6
- Other case reports have demonstrated that 20 mL or less of rapid air intake may result in fatal embolism.7
- In general, air volume greater than 50 mL is considered potentially lethal.8
Clinical presentation of air embolism
VAE may have cardiovascular, pulmonary, and neurologic effects, dependent on the rate and entrained volume of air.1 Rapid bolus injection may result in precipitous cardiovascular collapse, whereas gradual accumulations (Figure 1: microbubbles) may go unnoticed.8 The Figure below illustrates the relation between acute embolism volume and clinical symptoms and signs.
References
- Mirski M.A., Lele A.V., M.D., Fitzsimmons L., Toung T.J.K. (2007). Diagnosis and Treatment of Vascular Air Embolism. Anesthesiology; 106: 164-177
- Oppenheimer M.J., Durant T.M., Lynch P. (1953). Body position related to venous air embolism and associated cardiovascular-respiratory changes. Am J Med Sci; 225: 362-73
- Alvaran S.B., Toung J.K., Graff T.E., Benson D.W. (1978). Venous air embolism: Comparative merits of external cardiac massage, intracardiac aspiration, and left lateral decubitus position. Anesth Analg; 57: 166-70
- Munson E., Merrick H.C. (1966). Effect of nitrous oxide on venous air embolism. Anesthesiology; 27: 783-7
- Toung T.J., Rossberg M.I., Hutchins G.M. (2001). Volume of air in a lethal venous air embolism. Anesthesiology; 94: 360-1
- Martland H.S. (1945). Air embolism: Fatal air embolism due to powder insufflators used in gynecological treatments. Am J Surg; 68: 164-9
- Muth C.M., Shank E.S. (2000). Gas embolism. N Engl J Med; 342 (7): 476-482
- Cook L.S. (2013). Infusion-Related Air Embolism. Journal of Infusion Nursing; 36 (1): 26-36
Central venous access is invaluable in the treatment of hospitalized patients and a commonly performed procedure.
- Approximately eight percent of hospitalized patients require central venous access, i.e. more than five million central venous catheters are inserted in the United States each year.1,2
- Often patients in the intensive care unit (ICU) require central venous access. Roughly 60% of ICU patients have CVCs and 24% of non-ICU patients have CVCs.3
- Over 15 million catheter-days / year (i.e., the total number of days of exposure to CVCs among all patients in a selected population during a selected time period) are recorded in the ICU in the Unites States alone.4
- Despite the lower rate of CVCs on non-ICU wards, the overall number of CVCs outside the ICUs exceeds that of the ICUs.3
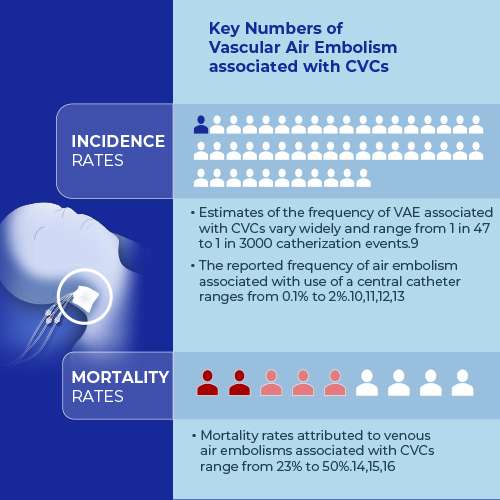
Central lines are not without risk and are associated with immediate, vascular, cardiac and pulmonary complications.5,6 Complications occur during catheter insertion, throughout the catheter dwell period, and at the time of removal.7 Incidence rates of catheter-related complications vary widely depending on the terminology and definition of complications, patient population, units of measurement, duration of catheterization and follow-up, catheter location, placement and care procedures, and diagnostic methods.8 The most common type of complication is catheter-related bloodstream infection (CRBSI). CRBSIs are reported with 4.3% to 26% of placed catheters.7 In comparison to CRBSIs the incidence rate of vascular air emboli (VAE) associated with CVCs are lower.
- Estimates of the frequency of VAE associated with CVCs vary widely and range from 1 in 47 to 1 in 3000 catherization events.9
- The reported frequency of air embolism associated with use of a central catheter ranges from 0.1% to 2%.10,11,12,13
According to a Pennsylvania Patient Safety Authority report about air embolism events,
- 41% of VAEs are associated with central venous access devices,
- 30% of VAEs are associated with surgical procedures,
- 24% of VAEs are associated with intravascular procedures and
- 5% of VAEs are associated with peripheral venous access devices.14
However, either because small amounts of air can go undetected as they often do not cause clinically significant consequences or because the diagnosis is easily missed, the true incidence of VAE is thought to be higher.13 While the frequency of this complication may be low, mortality rates attributed to venous air embolisms associated with CVCs range from 23% to 50%.14,15,16
Even the most conservative estimates (5 million CVCs per year in US, air embolus 0.1% of CVCs, and 23% mortality) indicate 1,150 deaths per year from this complication in the US alone.17
References
- Ruesch S., Walder B., Tramèr M.R. (2002). Complications of central venous catheters: internal jugular versus subclavian access--a systematic review. Crit Care Med; 30: 454
- McGee D.C., Gould M.K. (2003). Preventing complications of central venous catheterization. N Engl J Med; 348: 1123
- Climo, M. et al. (2003). Prevalence of the Use of Central Venous Access Devices Within and Outside of the Intensive Care Unit: Results of a Survey Among Hospitals in the Prevention Epicenter Program of the Centers for Disease Control and Prevention. Infection Control & Hospital Epidemiology; 24 (12): 942-945
- Mermel LA. (2000). Prevention of intravascular catheter-related infections. (Erratum: Ann Intern Med 133:395, 2000). Ann Intern Med 2000; 132: 391-402
- Kornbau C., Lee K.C., Hughes G.D., Firstenberg M.S. (2015). Central line complications. International Journal of Critical Illness and Injury Science; 5 (3): 170-178
- Patel A.R., Patel A.R., Singh S., SinghS., Khawaja I. (2019). Central Line Catheters and Associated Complications: A Review. Cureus; 11(5): e4717
- Napalkov P., Felici D.M., Chu L.K., Jacobs J.R, Begelman S.M. (2013). Incidence of catheter-related complications in patients with central venous or hemodialysis catheters: a health care claims database analysis. BMC Cardiovascular Disorders; 13 (86): 1-10
- Boersma R.S., Jie K.S., Verbon A., van Pampus E.C., Schouten H.C. (2008). Thrombotic and infectious complications of central venous catheters in patients with hematological malignancies. Ann Oncol; 19: 433-442
- Cook L.S. (2013). Infusion-Related Air Embolism. Journal of Infusion Nursing; 36 (1): 26-36
- Gordy S., Rowell S. (2013). Vascular air embolism. Int J Crit Illn Inj Sci;3 (1): 73-76
- Scott W.L. (1988). Complications Associated with Central Venous Catheters: A Survey. Chest; 94 (6): 1221-1224
- Vesely T.M. (2001). Air Embolism during Insertion of Central Venous Catheters. Journal of Vascular and Interventional Radiology; 12 (11): 1291-1295
- Bulsara K.R., MD, Lee S., Calafiore R. (2020). Commentary: Air Bubbles in Infusion: An Easily Avoidable Potential Complication. Operative Neurosurgery; 18 (2): E59-E60
- Feil M. (2015). Preventing central line air embolism. Am J Nurs; 115 (6): 64-9.
- Heckmann J.G. et al. (2000). Neurologic manifestations of cerebral air embolism as a complication of central venous catheterization. Crit Care Med; 28(5): 1621-5
- Kashuk J.L., Penn I. (1984). Air embolism after central venous catheterization. Surg Gynecol Obstet; 159: 249-52
- Patientsafe (2021) Central Line Air Emboli: one death every day? from https://patientsafe.wordpress.com/2016/11/14/central-line-air-embolus-one-death-every-day/ [accessed on 03_02_2021]
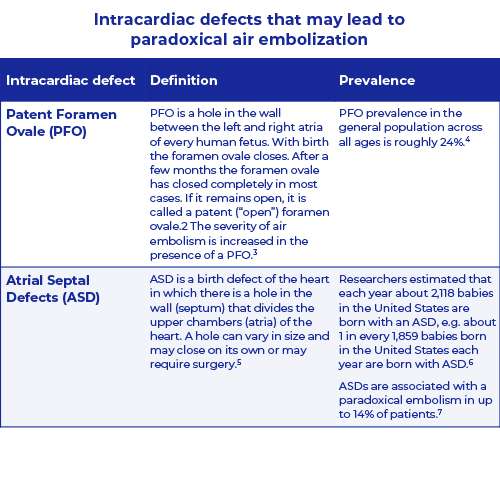
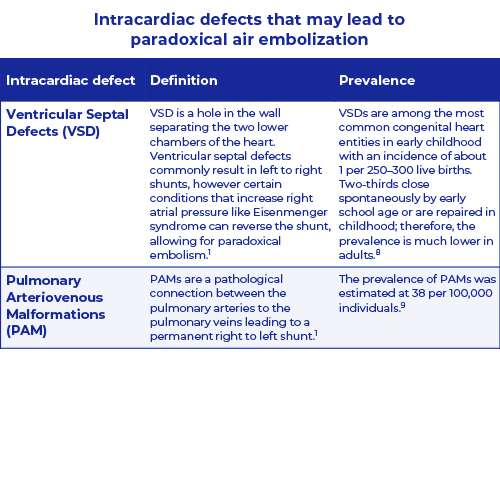
Paradoxical Embolism (PDE) occurs when a thrombus crosses an intracardiac defect into the systemic circulation. The emboli is usually a blood clot but maybe also a fat particle, amniotic fluid, tumor or air.1
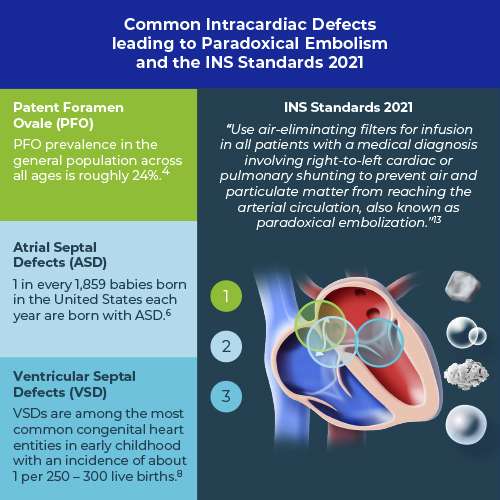
There are four intracardiac defects: Patent Foramen Ovale (PFO), Atrial Septal Defect (ASD), Ventricular Septal Defect (VSD) and Pulmonary Arteriovenous Malformation (PAM).
For more information see table and figure below.
Specifically, the presence of a PFO is related to arterial air embolization following intravenous air.10 Patent Foramen Ovale (PFO) is a common abnormality affecting between 20% and 34% of the adult population.11 Heckmann reported a PFO in 40% of cases with cerebral air embolism in association with central venous cannulation.12
US guidelines recommend IV filtration to mitigate the risk of Paradoxical Embolism
In 2021 the Infusion Nursing Society (INS) states:
“Use air-eliminating filters for infusion in all patients with a medical diagnosis involving right-to-left cardiac or pulmonary shunting to prevent air and particulate matter from reaching the arterial circulation, also known as paradoxical embolization. Hypercoagulable states and increased right heart pressure are associated with increased risk of paradoxical embolization.”13
References
- Hakman E.N., Cowling K.M. (2021). Paradoxical Embolism. [Updated 2020 Sep 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470196/
- American Heart Association (2021). Patent Foramen Ovale (PFO). [Updated 2017 March 31]. Available from: https://www.heart.org/en/health-topics/congenital-heart-defects/about-congenital-heart-defects/patent-foramen-ovale-pfo
- Cook L.S. (2013). Infusion-Related Air Embolism. Journal of Infusion Nursing; 36 (1): 26-36
- Koutroulou I. et al. (2020). Epidemiology of Patent Foramen Ovale in General Population and in Stroke Patients: A Narrative Review. Front Neurol; 11 (281)
- CDC (2021). Facts about Atrial Septal Defect. [Updated 2020 November 17]. Available from: https://www.cdc.gov/ncbddd/heartdefects/atrialseptaldefect.html
- Mai C.T. et al. (2019). National population-based estimates for major birth defects, 2010-2014. Birth Defects Res; 111 (18): 1420-1435
- Bannan A., Shen R., Silvestry F.E., Herrmann H.C. (2009). Characteristics of adult patients with atrial septal defects presenting with paradoxical embolism. Catheter Cardiovasc Interv; 74(7): 1066-9
- Kochav J. (2018) Ventricular Septal Defect. In: DeFaria Yeh D., Bhatt A. (eds) Adult Congenital Heart Disease in Clinical Practice. In Clinical Practice. Springer, Cham. https://doi.org/10.1007/978-3-319-67420-9_5
- Nakayama M. et al. (2012). Prevalence of pulmonary arteriovenous malformations as estimated by low-dose thoracic CT screening. Intern Med; 51 (13): 1677-81
- Wilkins R.G., Unverdorben M. (2012). Intravenous Infusion of Air. Journal of Infusion Nursing; 35 (6): 404-408
- Giblett J.P., Abdul-Samad O., Shapiro L.M., Rana B.S., Calvert P.A. (2019). Patent Foramen Ovale Closure in 2019. Interv Cardiol;14 (1): 34-41
- Heckmann J.G. et al. (2000). Neurologic manifestations of cerebral air embolism as a complication of central venous catheterization. Crit Care Med; 28 (5): 1621-1625
- Gorski L.A. et al. (2021). Infusion Therapy Standards of Practice, 8th Edition. J Infus Nurs; 01(44): S1-S224
Have you ever seen air bubbles eliminated by a Pall IV in-line filter?
Our air-eliminating filters prevent air from entering the vascular system of adult, pediatric, and neonate patients. Results from internal studies demonstrate that Pall filters can eliminate entrained air in both a vertical and horizontal position.1
Watch this video and see how air bubbles are eliminated by our IV in-line filters.
Statements regarding IV in-line filters as a preventive strategy for eliminating air in infusion lines:
- “Although there are no data available from adequately designed clinical studies, the safest available approach is the use of an air elimination filter.”2
- “Use an air-eliminating filter on infusion tubing sets whenever appropriate.”3
References
- Amanda S. (2010). Air Elimination Capabilities of the Pall Lipipor™ TNA2 Filter for Parenteral Nutrition. Pall Technical Report: # 10.3992
- Wilkins R.G., Unverdorben M. (2012). Intravenous Infusion of Air. Journal of Infusion Nursing; 35 (6): 404-408
- Feil M. (2012). Reducing Risk of Air Embolism Associated with Central Venous Access Devices. Pennsylvania Patient Safety Authority; 9 (2): 58-65
Preventing the entrance of air into the patient’s circulatory system can result in tangible budget savings for the healthcare provider.
- Vascular air embolism (VAE) illustrates a significant financial burden for hospitals. VAE complications costs the healthcare system, on average, $66,007 per incident.1-3
- In the case of severe multiple complications which may require full ICU treatment, a healthcare provider may save up to 56,670 € per prevented event.4-8
Centers for Medicare and Medicaid Services includes air embolism as a preventable and non-reimbursable event in the United States
A hospital acquired condition (HAC) is one of several medical diagnoses a patient can develop during a hospital stay that was not present on admission.9
- In 2008, a provision of the Deficit Reduction Act of 2005 known as Medicare “Nonpayment” went into effect, eliminating reimbursement for the marginal costs of preventable HACs, including air embolism.10
- In 2015, the federal HAC Reduction Program requires the Centers for Medicare & Medicaid Services to reduce payments by 1% for hospitals in the top quartile of risk adjusted national HAC scores.11
Hospitals may consider the use of IV in-line filters to prevent the risk of air embolism associated with central venous access devices.
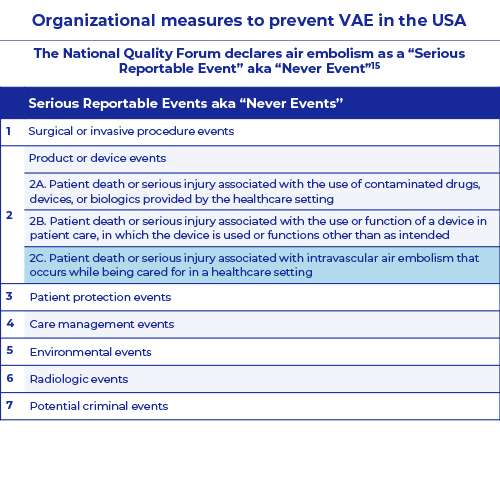
The National Quality Forum declares air embolism as a “Serious Reportable Event” aka “Never Event”
The National Quality Forum (NQF) is a not-for-profit, nonpartisan, membership-based organization that works to catalyze improvements in healthcare. Preventing adverse events in healthcare is central to NQF’s patient safety efforts. The term "Never Event" was first introduced by the NQF, in reference to particularly shocking medical errors that should never occur.12 To ensure that all patients are protected from injury while receiving care, NQF has developed and endorsed a set of Serious Reportable Events (SREs) aka “Never Events”. This set is a compilation of serious, largely preventable, and harmful clinical events, designed to help the healthcare field to assess, measure, and report performance in providing safe care.13
Vascular air embolism is considered as a serious reportable event according to the National Quality Forum 2011 update.14 Hospitals, outpatient/office-based surgery centers, ambulatory practice settings/office-based practices, long-term care/skilled nursing facilities may consider the use of IV in-line filters to prevent the risk of air embolism.
References
- Rowland HT. (2009). When never happens: Implications of Medicare’s never event policy. Marquette Elder’s Advi; 10: 341-82
- Bhananker S.M. et al. (2009). Liability related to peripheral venous and arterial catheterization: A closed claims analysis. Anesth Analg; 109: 124-9
- Domino K.B. et al. (2004). Injuries and liability related to central vascular catheters: A closed claims analysis. Anesthesiology; 100: 1411-8
- Mirski et al.2007, Perdue 2001, Wittenberg 2006 Diagnosis and treatment of vascular air embolism. Anesthesiology 2007; 106(1): 164-77
- Josephson DL. Risks, complications, and adverse reactions associated with intravenous infusion therapy. In: Josephson DL. Intravenous infusion therapy for medical assistants.The American association of Medical Assistants. Clifton Park: Thomson Delmar Learning 2006; 56-82
- Souders JE. Pulmonary air embolism. J Clin Monit Comput 2000; 16(5-6): 375-83
- Lamm G, Auer J, Punzengruber C, Ng CK and Eber B. Intracoronary air embolism in open heart surgery – an uncommon source of myocardial ischaemia. Int J Cardiol 2006; 112(3): 85-6
- Demaerel P, Gevers AM, De Bruecker Y, Sunaert S and Wilms G. Gastrointest Endosc. Stroke caused by cerebral air embolism during endoscopy 2003; 57(1): 134-5
- Center for Medicare and Medicaid Services. (2020). Publicly Reported DRA HAC Measures - Frequently Asked Questions from https://www.cms.gov/files/document/frequently-asked-questions-publicly-reported-deficit-reduction-act-dra-hospital-acquired-condition.pdf [accessed 02/23/2021]
- Kornkven A. (2020). The Impact of Medicare Nonpayment: A Quasi-Experimental Approach from https://sites.duke.edu/djepapers/files/2020/06/audreykornkven-dje.pdf [accessed 02/23/2021]
- Mariano E Menendez M.E. and David Ring D. (2015). Do hospital-acquired condition scores correlate with patients' perspectives of care? Qual Manag Health Care; 24(2): 69-7
- Patient Safety Network (2021). Never Events from https://psnet.ahrq.gov/primer/never-events [accessed 02/23/2021]
- National Quality Forum (2021). Serious Reportable Events from http://www.qualityforum.org/topics/sres/serious_reportable_events.aspx#:~:text=Serious%20Reportable%20Events%20aka%20%22Never%20Events%22&text=This%20set%20is%20a%20compilation,performance%20in%20providing%20safe%20care [accessed 02/23/2021]
- National Quality Forum (2021). List of Serious Reportable Events (aka SRE or "Never Events") from http://www.qualityforum.org/Topics/SREs/List_of_SREs.aspx [accessed 02/23/2021]
The Infusion Nurses Society (INS) and the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) are recommending in-line filtration as a preventive strategy to mitigate the risk of air embolism.1,2
INS recommends the use of IV in-line filters1
- for solutions and medications to reduce microbubbles (<1 mm in diameter) of air and
- for all patients with a medical diagnosis involving right-to-left cardiac or pulmonary shunting to prevent air and particulate matter from reaching the arterial circulation, also known as paradoxical embolization.
A.S.P.E.N. recommends the use of IV in-line filters2
- for Parenteral Nutrition (PN) administration to reduce the potential for patient harm due to particulates, microprecipitates, microorganisms, and air emboli.
References
- Gorski L.A. et al. (2021). Infusion Therapy Standards of Practice, 8th Edition. J Infus Nurs; 01(44): S1-S224
- Ayers P. et al. (2014) A.S.P.E.N. Parenteral Nutrition Safety Consensus Recommendations. Journal of Parenteral and Enteral Nutrition; 38 (3): 296-333
Our highly skilled technical experts in our “Scientific Laboratory Services” (SLS) are here to support you and offer advice on optimal intravenous filtration and infusion solutions or to perform drug compatibility studies.
Our Clinical Specialists support customers who wish to implement Pall intravenous, breathing and gas filtration devices. They implement and evaluate our products in hospitals at the patient’s bedside and advise on any problems that might arise.
You can reach them easily via your local sales rep or through customer services.